News
Scheme’s success at stopping mums-to-be smoking
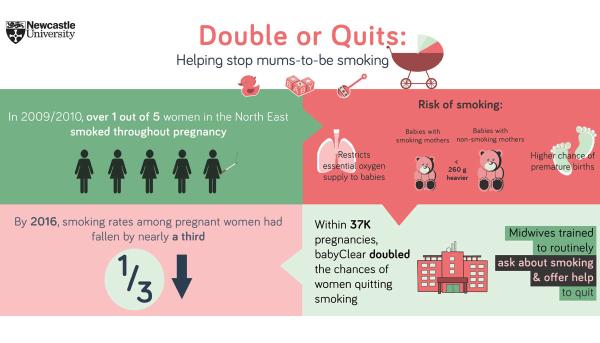
Pregnant women are almost twice as likely to quit smoking if they are supported from their first midwife appointment – and then are more likely to have heavier, healthier babies.
Academics from Fuse, the Centre for Translational Research in Public Health, based at Newcastle University and Teesside University evaluated the “BabyClear” programme which follows the National Institute for Health and Care Excellence (NICE) guidance around smoking in pregnancy by screening all pregnant women for smoking using carbon monoxide monitoring.
Any woman still smoking when she first saw a midwife, at around eight weeks into pregnancy, was given information about the risks to their unborn baby. She was then put in contact with agencies who could help her quit.
Publishing today in Tobacco Control, the research team report that in the study of 40,000 mothers-to-be, the number of women helped to stop smoking almost doubled.
Dr Ruth Bell, senior lecturer in the Institute of Health and Society at Newcastle University, who led the study, said: “This shows that if we help make it routine for midwives to ask about smoking and screen every mother-to-be for carbon monoxide, we can double the number of women who quit smoking in pregnancy and substantially increase the number of healthy babies.”
The team found the women who did not smoke in pregnancy, went on to have babies that were more than half-a-pound heavier (260 grams or 0.57lb) at full term, than those who continued to smoke.
Even women who quit smoking during their pregnancy were shown to have heavier babies (by around 210 grams or 0.46lb) than those of mothers who smoked throughout pregnancy. This is an indicator of a healthier infant that is likely to need less medical help.
Effective
The large study in NHS maternity units across the north east of England, included 10, 594 women who were smokers. Every woman was offered carbon monoxide (CO) monitoring and anyone with high carbon monoxide readings, indicating smoking, was routinely referred to Stop Smoking Services within 24 hours, where they received help to stop from a trained smoking cessation adviser.
Dr Bell said: “Training midwives particularly on how to start a conversation about smoking, along with providing clear routes for women to get support to help stop smoking, ensured that national guidance was followed. This package proved to be highly effective in helping mothers to stop smoking, equivalent to nearly 100 extra quitters per year in a maternity unit delivering 3,000 babies.”
The study was funded by the NIHR School for Public Health Research (SPHR) and Fuse, the Centre for Translational Research in Public Health.
Findings
The study examined the records of 37,726 births of single babies across the North East, including 10,594 to mothers who smoked during pregnancy. The authors report that the referral rate more than doubled (2.5 times higher) across all the trusts in the first three months after the introduction of the new approach.
The introduction of the programmes was associated with a substantial increase in quitting during pregnancy, and quitting was associated with referral to stop smoking services. Further analysis of birthweight revealed that babies were significantly heavier if a mother quit smoking during pregnancy.
Professor Eugene Milne, a co-author of the study and Director of Public Health at Newcastle City Council, said: “It is hard to overstate the impact that being smoke free can have on babies, mothers and families.
“Reducing smoking reduces the risk of stillbirth, low birth weight, and of problems with health not only in childhood but into adult life and even old age. There is clear evidence that heavier babies have lower rates of heart disease in later life.
“This new study provides important evidence that giving the right care to help pregnant mothers quit smoking is an effective and important intervention, and provides the information and help that mothers want.
“We are working to ensure that all prospective mothers receive this standard of care and support in Newcastle and the North East.”
Economic analysis revealed that the additional cost of the intervention per delivery was £31.
The work was possible as the North East has a regional approach to reducing smoking during pregnancy, embedding NICE guidance using the BabyClear approach developed by Improving Performance in Practice (iPiP). This was rolled out in the North East by Fresh, the North East’s regional tobacco control programme, working with all of the North East's hospital foundation trusts and Stop Smoking Services.
Smoking at the time of delivery rates have fallen in the North East since 2009/10 when 22.2% of women smoked at the time they gave birth, down to 16% in 2016.
Reducing harm from tobacco
Ailsa Rutter, Director of Fresh, which supported the introduction of the approach across the region said: “These findings and the drastic decline in smoking in pregnancy in the North East by around a third since 2009 shows the vital role the NHS can play in reducing harm from tobacco. But it is vital this work continues.
“There is a lack of awareness around just how smoking harms unborn babies and midwives played an important role in communicating this. Women overwhelmingly supported this approach, even if some initially found the facts shocking.
“There has also been demand for this approach to be rolled out nationally by leads from the national Smoking in Pregnancy Challenge Group, a coalition working to reduce the harm caused by tobacco.”
Professor Linda Bauld, Co-Chair of the Smoking in Pregnancy Challenge Group and Professor of Health Policy at the University of Stirling said: "The North East of England has taken a lead in implementing recommendations from NICE and the Smoking in Pregnancy Challenge group, and progress achieved is impressive.
“These results show the vital role health professionals can play when they raise the issue of smoking. These changes have undoubtedly saved lives and have implications that go beyond pregnancy for the role front line NHS professionals can play.”
Dr Bell adds: “Our analysis shows that by improving the links between midwives and smoking cessation services we can really help mothers give their babies the best start in life.”
REFERENCE: Evaluation of a complex healthcare intervention to increase smoking cessation in pregnant women: interrupted time series analysis with economic evaluation. Ruth Bell et al. Tobacco Control. Doi: 10.1136/tobaccocontrol-2016-053476
Case study: Melanie’s story
 Melanie Snowdon, 40, from South Shields, welcomed her fifth child, Faith (both pictured right), to the world in March. When she found out she was expecting she sought support from her local stop smoking service to quit tobacco for the good of her unborn child. She’s continued to be smoke free following the birth and is confident that she’ll remain that way in the future.
Melanie Snowdon, 40, from South Shields, welcomed her fifth child, Faith (both pictured right), to the world in March. When she found out she was expecting she sought support from her local stop smoking service to quit tobacco for the good of her unborn child. She’s continued to be smoke free following the birth and is confident that she’ll remain that way in the future.
“I was about 17 when I started smoking. In those days everybody smoked, we knew it was bad but you don’t think about that when you’re a teenager. On average I smoked about 20 - 30 a day and it wasn’t until I was pregnant with my fifth child that I stopped.
“I smoked through my first four pregnancies and there were no issues, I had four healthy babies. There was a big gap in between my first four and my youngest.
“Not long after I married my husband, we fell pregnant again. I decided that I needed to quit smoking as my husband doesn’t smoke and doesn’t like it.
“The thing that really hit home for me was when the midwife at hospital showed me how much carbon monoxide was in my breath and explained how smoking starves the baby of oxygen.
“I was referred to my local stop smoking service and, at first, I was very sceptical. I used patches, sprays and an ecig for a little bit too and I managed to come off the cigarettes completely after seven weeks.
“I couldn’t quite believe the difference in weight, my daughter was 9lbs 12oz whereas all my other children were much lighter. I never believed that smokers had smaller babies.
“I wasn’t sure how I would do after my daughter was born but I’m still off the cigarettes and I can’t see myself going back. I still carry a spray in my bag just in case but the thought and the smell of smoking really puts me off.
“My husband has said he is really proud of me because he thought once the baby was born I would have started again.
“I would encourage other mums to give it a try - it doesn’t cost anything. I smoked for so many years and would never have thought I would be able to stop but I did.”
Last modified: Thu, 16 Feb 2017 09:34:26 GMT
